Globally recognised academic research and clinical practice experts contribute insights
WATERLOO, Ontario, September 30, 2020—The Centre for Ocular Research & Education (CORE) has published issue number 55 of its free online education magazine, Contact Lens Update. The latest edition reviews a number of new publications focused on how the efficacy of myopia management interventions varies with the dose of treatment used.

Mark Bullimore, internationally recognised scientist, speaker and educator, provides an extensive review of the implications of the results from the recently-publicized BLINK study. He describes how the findings fit into the overall understanding of myopia management, and how eye care practitioners can make use of them in practice.

Philip Cheng, clinical director of the Myopia Clinic Melbourne, offers two contributions. He builds on the BLINK study results, reviewing evidence of a dose-dependent response in other myopia management interventions. He then draws on his considerable practical experience to demonstrate how to apply this information directly to the choice of recommended treatments.
The theme of a dose-dependent response is also covered in the issue’s conference highlight. A study conducted by Jan Roelof Polling and colleagues in a myopia control clinic in the Netherlands confirms the previously reported relationship between improved control of axial length change and higher concentrations of atropine.
“This new content exemplifies our aims for Contact Lens Update—direct translation of current research into clinical application,” said Karen Walsh, the magazine’s editor and CORE clinical scientist and professional education team leader. “I am sure many eye care practitioners interested in myopia management will find this information especially useful when advising children and their parents on available options.”
Published six times per year, Contact Lens Update provides a global platform for unbiased clinical insights based in current research. Since 2011, each issue has provided dependable and up-to-date ocular health information for more than 60,000 leading eye care professionals.
In addition to a complete archive of back issues, ContactLensUpdate.com offers a resource library that provides no-cost professional tools, patient resources, images and video. It also houses complimentary technical training videos produced by International Association of Contact Lens Educators, plus an industry glossary. Industry professionals can access the latest issue directly from ContactLensUpdate.com or quickly sign up for email receipt of future issues.
The publication receives support from the educational arms of Alcon, CooperVision, and Johnson & Johnson Vision.
# # #
About the Centre for Ocular Research & Education (CORE)
The Centre for Ocular Research & Education (CORE) was established in 1988 at the University of Waterloo’s School of Optometry & Vision Science. Over the next three decades, the organization evolved from a three-person operation into a thriving hub of basic and applied research, collaborating with sponsors, agencies and academia on advanced biosciences, clinical research and education. Its uncompromising independence and results of the highest quality have been at the heart of many of the most prominent advances in eye health. Today, its approximately 50-person team serves a range of ophthalmic sectors, including medical devices, ocular pharmaceuticals, digital technology and others, with a focus on the anterior segment. For more information, please visit core.uwaterloo.ca.
MEDIA CONTACTS
Aimee J. Lewis or Mike McDougall, APR, Fellow PRSA, McDougall Communications for CORE
aimee@mcdougallpr.com +1.585.414.9838 | mike@mcdougallpr.com +1.585.545.1815






 “In less than a month from when we first described MADE in
“In less than a month from when we first described MADE in 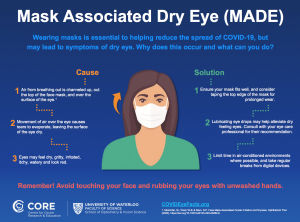
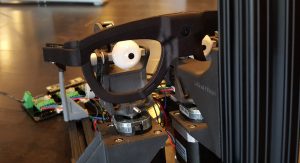 AdHawk has incorporated the OcuBlink eyeballs into its round-the-clock robotic testing system to evaluate its algorithms and new devices, such as AR/VR glasses, with a high degree of replicability. This precision is required for the company’s unique microsystems that take and process thousands of measurements every second, allowing on-the-fly velocity calculations with unprecedented resolution. Since velocity profiles of saccades (the rapid involuntary movements of the eye) are highly consistent, AdHawk’s proprietary algorithms can predict where a user will look.
AdHawk has incorporated the OcuBlink eyeballs into its round-the-clock robotic testing system to evaluate its algorithms and new devices, such as AR/VR glasses, with a high degree of replicability. This precision is required for the company’s unique microsystems that take and process thousands of measurements every second, allowing on-the-fly velocity calculations with unprecedented resolution. Since velocity profiles of saccades (the rapid involuntary movements of the eye) are highly consistent, AdHawk’s proprietary algorithms can predict where a user will look.

 WATERLOO, Ontario, May 20, 2020—“
WATERLOO, Ontario, May 20, 2020—“