Despite Widespread Global Slowdowns in Clinical Research, CORE Perseveres to Reach New Publishing Milestone
WATERLOO, Ontario, December 17, 2021—In a year like no other, the Centre for Ocular Research & Education (CORE) has published a record 66 scientific and clinical educational papers on topics that advance academic and clinical knowledge in optometry and ophthalmology. The organization today announced its “Top 10 of 2021” list, designating particularly valuable works for the global eye care community.
As the COVID-19 pandemic kept workplaces, schools and businesses shuttered worldwide, clinical research was severely impacted. Early pandemic reports indicated that more than 65% of science and technology-related research was paused or delayed due to COVID-related closures. Yet even in the midst of widespread disruption, CORE continued to publish and present topics essential for both current practice and future ophthalmic progress.
“We found a way to overcome another year of pandemic challenges to further evolve and advance ocular science and education, thanks to my incredible colleagues at CORE and our collaborators around the globe,” says CORE Director Lyndon Jones, PhD, DSc, FCOptom, FAAO. “With our record publication volume, it would be easy to overlook some of the most critical pieces of work. The top 10 selections underscore the highest-potential research for eye care professionals, spanning topics such as dry eye, drug delivery, myopia control, eye simulation models, and future contact lens technologies.”
Papers making the “top 10” for 2021 include:
- Ocular health of children wearing daily disposable contact lenses over a 6-year period (Woods J, et al.), Contact Lens & Anterior Eye
Fitting pre-teen children with soft contact lenses has become more prevalent worldwide, driven largely by using contact lenses for myopia control. Practitioners are keen to understand how these young eyes adapt to full-time lens wear. This manuscript presents the physiological data from a six-year daily disposable soft lens wearing, global, multi-site trial; CORE was the largest clinical site in this trial. This is the longest prospective contact lens trial reported to date. Children aged 8-12 years were enrolled and with 92 completing the study, the data is representative of 653 lens wearing years. There were no contact lens related serious adverse events. Careful slit-lamp observations were similar after six years to the baseline values. The results support that children of this age can successfully wear daily disposable soft contact lenses with minimal impact on ocular physiology. https://doi.org/10.1016/j.clae.2020.11.011
- Lysozyme Deposition on Contact Lenses in an In Vitro Blink-Simulation Eye Model Versus a Static Vial Deposition Model (Chan V, et al.), Eye & Contact Lens
CORE has considerable expertise in quantifying protein deposition on contact lenses. This paper compares lysozyme deposition on contact lenses using two in vitro models; a static vial versus a sophisticated in vitro eye model with a blinking mechanism. This study showed that the in vitro blink model can be tuned to mimic quantitative lysozyme deposition data from ex vivo studies, which may provide new opportunities for developing and optimizing other ocular models. https://doi.org/10.1097/ICL.0000000000000784
- All soft contact lenses are not created equal (Efron N, et al.), Contact Lens & Anterior Eye
Soft contact lenses that have been carefully prescribed by eye care practitioners are sometimes arbitrarily substituted for alternative lenses in the mistaken belief that there is essentially no difference between various lens types. CORE Director Lyndon Jones is a contributor to this broad-ranging, evidence-based review that considers potential complications induced by inappropriate substitution without practitioner oversight. Substitution of 15 of the 16 lens properties considered was found to be related to potential sources of patient dissatisfaction and adverse ocular events. The conclusions presented confirm that a substituted lens may have properties that result in undesirable consequences in respect of vision, ocular health and comfort and that unqualified, unsupervised lens substitution should be avoided. https://doi.org/10.1016/j.clae.2021.101515
- Contact lens technologies of the future (Jones L, et al.), Contact Lens & Anterior Eye
Contact lenses in the future will likely have functions other than correction of refractive error. In this extensive review, CORE’s Lyndon Jones and Chau-Minh Phan and colleagues from around the globe report on the use, or potential use, of contact lenses for a wide-range of novel functions. The potential for contacts to be used to detect systemic and ocular surface diseases, treat and manage various ocular conditions and as devices that can correct presbyopia, control the development of myopia or be used for augmented vision are described in detail in the most far-reaching report of its kind to-date. https://doi.org/10.1016/j.clae.2021.02.007
- Development of an In Vitro Blink Model for Ophthalmic Drug Delivery (Phan C, et al.), Pharmaceutics
Successful drug therapy via topical ophthalmic administration requires overcoming multiple physical challenges. However, advancements in biomaterials and their application has led to innovative approaches in surmounting these challenges. This paper from the OcuBlink team at CORE describes the development of an eye model for testing drug release from a contact lens on the eye, which allows us to better predict the on-eye performance of ophthalmic formulations and devices. This, in turn, could lead to informing the direction for industry R&D and the development of improved products. https://doi.org/10.3390/pharmaceutics13030300
- Bulbar redness and dry eye disease: comparison of a validated subjective grading scale and an objective automated method (Schulze M, et al.), Optometry & Vision Science
The number of patients reporting symptoms of dry eye has been increasing steadily, particularly during digital device use. While the majority of diagnostic tests for dry eye focus on tear film assessments, increased levels of ocular redness have also been associated with dry eye. In their study, Marc Schulze and colleagues from CORE used the Oculus K5M and the validated bulbar redness (VBR) scale to evaluate whether objectively and subjectively graded ocular redness levels can be used to discriminate between dry eye and non-dry eye patients. Their findings showed that assessing ocular redness by zone, after asking patients to change their gaze to expose larger conjunctival areas compared to en-face assessments, is of high relevance for redness assessments related to dry eye. This is an assessment that can easily be included into the routine biomicroscopy exam in clinical practice and may be helpful to assess dry eye treatment efficacy. https://doi.org/10.1097/opx.0000000000001638
- The Impact of Incubation Conditions on in Vitro Phosphatidylcholine Deposition on Contact Lens Materials (Walther H, et al.), Optometry & Vision Science
Previous work has suggested that more hydrophobic materials (such as silicone hydrogels) may be prone to adsorbing lipids to a greater extent than conventional hydrogel materials. However, deposition of all lipids may not necessarily be detrimental, as lipids such as phosphatidylcholine are important stabilizing components of the tear film. This research by CORE researcher Hendrik Walther and colleagues explores various aspects of lipid uptake that may impact contact lens performance. The results provide important information regarding how to evaluate lipid uptake when undertaking in vitro studies, with length of incubation, lipid concentration in the doping solution and the frequency of replenishment of the lipids all impacting the data obtained. https://doi.org/10.1097/opx.0000000000001680
- Clinical practice patterns in the management of dry eye disease: A TFOS international survey (Wolffsohn J, et al.), Ocular Surface
Dry eye disease is one of the most common conditions encountered in eye care. In this paper, CORE was part of an international survey effort to examine the clinical practice patterns of optometrists and ophthalmologists from 51 countries. This paper found that management strategies depended highly on severity and subtype, and on the country. This information allows practitioners from local regions to compare their practice with their peers and identifies potential areas to optimize patient treatment. https://doi.org/10.1016/j.jtos.2021.04.011
- Optimization of goblet cell density quantification methods (Yang M, et al.), Experimental Eye Research
Goblet cells play a vital role in maintaining ocular surface homeostasis, however, there is no standard method for their quantification. This paper investigated the nuances and various methods for quantifying goblet cell density and was achievable only through a collaboration between the clinical and basic science expertise at CORE. This type of translational research is necessary to advance the clinical diagnosis of dry eye disease at a fundamental level. https://doi.org/10.1016/j.exer.2021.108607
- Uptake and release of a multipurpose solution biocide (MAP-D) from hydrogel and silicone hydrogel contact lenses using a radiolabel methodology (Yee A, et al.), Eye & Contact Lens
Multipurpose contact lens solutions contain a variety of biocides that ensure safe disinfection of the lenses overnight. However, their uptake into soft lenses during the overnight soak time and the subsequent release onto the ocular surface during wear have been linked to several complications. Determination of this uptake and release is complicated, as the amounts are small and studying this issue has been dogged by the complexity of the analytical methods required. Alan Yee, a CORE PhD student, reports on a methodology evaluating the uptake and release of a common biocide (myristamidopropyl dimethylamine; MAP-D) using a novel radiolabelled method. The data showed that silicone hydrogel materials absorbed greater amounts of MAP-D compared to hydrogels, but the hydrogel materials released the greatest amount of the biocide. Radioactive labelling of biocides offers a highly sensitive method of assessing the uptake and release profiles of biocides to CL materials. https://doi.org/10.1097/icl.0000000000000724
CORE offers a searchable database of its nearly 2,500 peer-reviewed papers, professional articles, continuing education presentations, and scientific presentations dating back to the early 1980s. That resource is available at https://core.uwaterloo.ca/publications/.
###
About the Centre for Ocular Research & Education (CORE)
The Centre for Ocular Research & Education (CORE) – formerly known as the Centre for Contact Lens Research – was established in 1988 at the University of Waterloo’s School of Optometry & Vision Science. Over the next three decades, the organization evolved from a three-person operation into a thriving hub of basic and applied research, collaborating with sponsors, agencies and academia on advanced biosciences, clinical research and education. Its uncompromising independence and results of the highest quality have been at the heart of many of the most prominent advances in eye health. Today, its approximately 50-person team serves a range of ophthalmic sectors, including medical devices, ocular pharmaceuticals, digital technology and others, with a focus on the anterior segment. For more information, please visit core.uwaterloo.ca.
MEDIA CONTACTS
Aimee J. Lewis or Mike McDougall, APR, Fellow PRSA
McDougall Communications for CORE
aimee@mcdougallpr.com +1.585.414.9838 | mike@mcdougallpr.com +1.585.434.2150










 “Rosa’s work on improving the clinical efficacy of specialty lenses through optimized design and auxiliary technologies—especially for myopia control and visual rehabilitation—is a natural fit with CORE’s growing work in these sectors,” said Dr. Lyndon Jones, CORE’s director.
“Rosa’s work on improving the clinical efficacy of specialty lenses through optimized design and auxiliary technologies—especially for myopia control and visual rehabilitation—is a natural fit with CORE’s growing work in these sectors,” said Dr. Lyndon Jones, CORE’s director.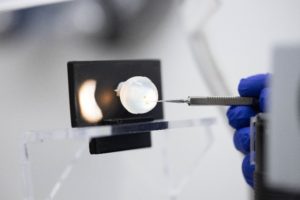 OcuBall feels like a human eye and simulates a realistic response to embedded foreign bodies, similar to those found in clinical environments. It replaces animal-based methods in optometry training environments while eliminating safety concerns related to handling, disposal and storage of biological tissue.
OcuBall feels like a human eye and simulates a realistic response to embedded foreign bodies, similar to those found in clinical environments. It replaces animal-based methods in optometry training environments while eliminating safety concerns related to handling, disposal and storage of biological tissue. OcuBall comes premade with metal steel particles inserted on the surface of the eye to provide a realistic, safe and inexpensive clinical scenario for the practice of foreign body removal. Over time, the metal pieces can rust and form a typical rust ring, just as they do in the human eye. Use in educational settings helps optometry students practice and gain confidence in the removal of materials from the eye.
OcuBall comes premade with metal steel particles inserted on the surface of the eye to provide a realistic, safe and inexpensive clinical scenario for the practice of foreign body removal. Over time, the metal pieces can rust and form a typical rust ring, just as they do in the human eye. Use in educational settings helps optometry students practice and gain confidence in the removal of materials from the eye.